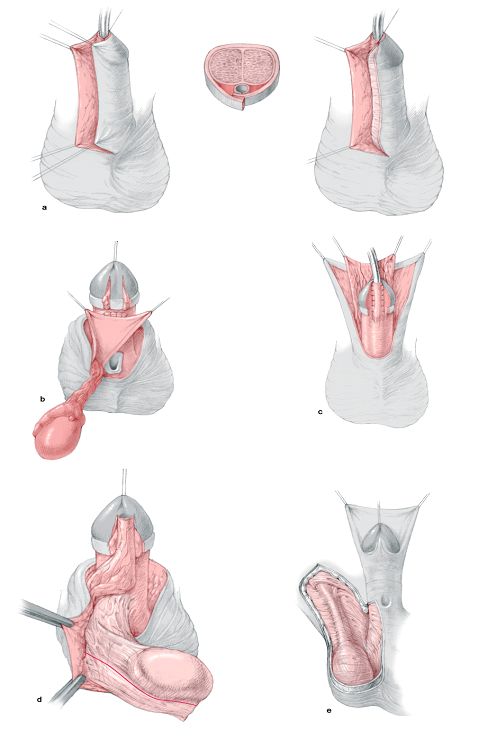
Onlay Island Flap
The Onlay Island Flap is ideal for patients with proximal hypospadias without deep Chordee. According to the author experience, most patients with proximal hypospadias have deep chordee that necessitates excision. However, recently, many surgeons prefer to perform dorsal placation if the chordee is less than 30o after skin degloving and preserve the urethral plate.
Operative steps
The tip of the neo-meatus is identified. This point is where the flat ventral surface of the glans begins to curve around the meatus. A midline vertical incision is made in the glans until the width of the glanular groove is adequate for the meatus. The vertical incision is left open without closure for secondary epithelialisation.
A subcoronal incision is made around the glans. The incision continues on either side of the urethral plate at the junction with the normal ventral skin, then up on either side of the glanular groove to the apex of the glansplasty.
The skin is degloved from distal to proximal close to the Buck's fascia preserving the arteries that constitute the pedicle to the preputial flap. The pedicle is then separated from the outer preputial skin in a plane just below the intrinsic blood supply of the outer prepuce. The elevation of the glans wings will permit them to be rotated around the urethroplasty.
A 1-cm wide onlay flap is prepared from the inner prepuce. The onlay flap is sutured into place beginning with the suture line underneath the pedicle utilizing running 7-0 polyglactin suture. The glans should be drawn together setting up the first stitch of the glansplasty ventrally at its apex.
The mobilized glans wings are rotated medially around the neo-urethra. Three transverse mattress sutures maintain firm approximation of the glanular wings in the midline.
Complications
Fistula, wound disruption, rotation, recurrent curvature occurs in 10 - 20 % of patients.
Two Stage repair
A small group of patients with severe proximal hypospadias, chordee, and a small phallus as well as patients with recurrent hypospadias and fibrous unhealthy skin may benefit from a two-stage procedure (Fig. 10).
In the first stage, a circumferential incision is made proximal to the coronal sulcus, the chordee is excised, and the penile shaft is de-golved. Penile straightening and removal of all chordee tissue must be confirmed by the use of the artificial erection test.
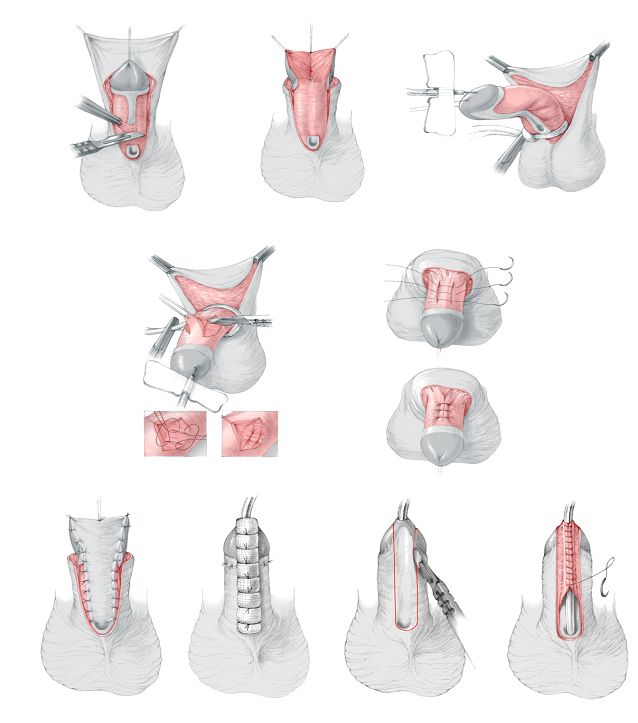 |
Fig. 10: Steps of two stage repair: identification of chordee, excision of ventral chordee and plication if needed. Coverage of raw surface with skin graft. Tubularisation as a final step