| |
Hypospadias Surgery
by Professor Ahmed T Hadidi
Professor of Paediatric Surgery, Heidelberg University, Germany
Professor of Paediatric and Plastic Surgery, Cairo University, Egypt
Hypospadias surgery has developed into a well defined art and science. Surgeons dealing with this anomaly should have a detailed understanding of the various basic surgical principles and experience with delicate, precise optically assisted techniques and maintain a clinical workload that is sufficient to obtain consistently good results.
Incidence
One in 300 boys has hypospadias. In the United States a study reported that hypospadias was the most common congenital anomaly among whites. The incidence has been rising during the 1970s and 1980s.
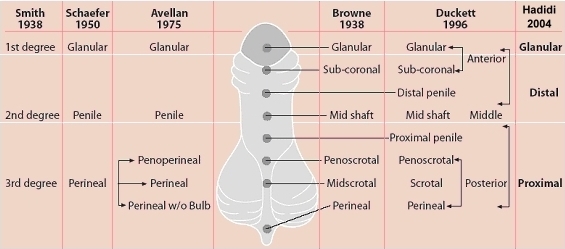
Classification
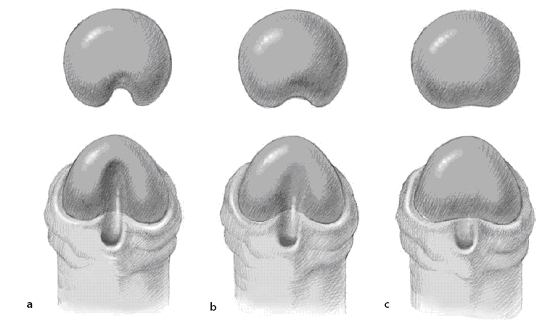
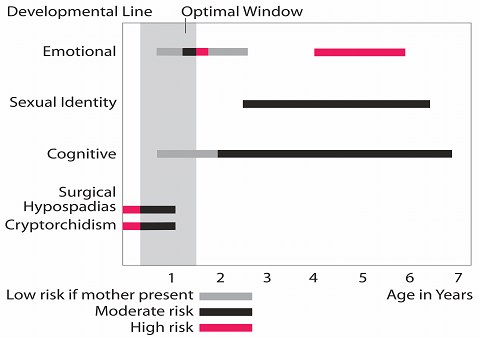
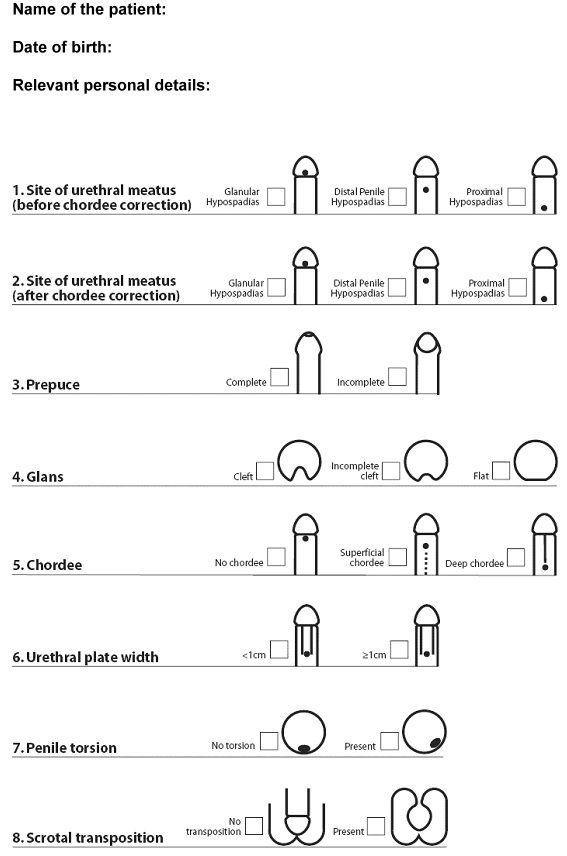
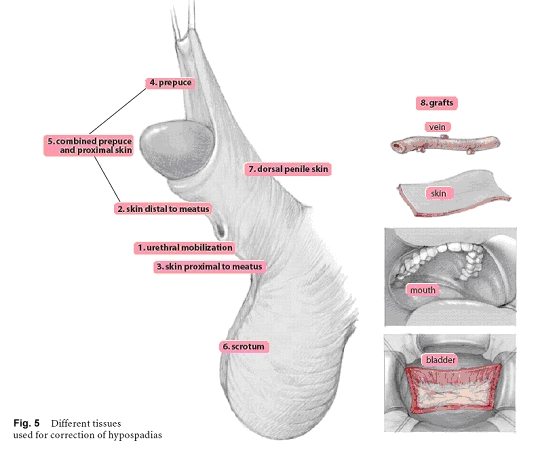
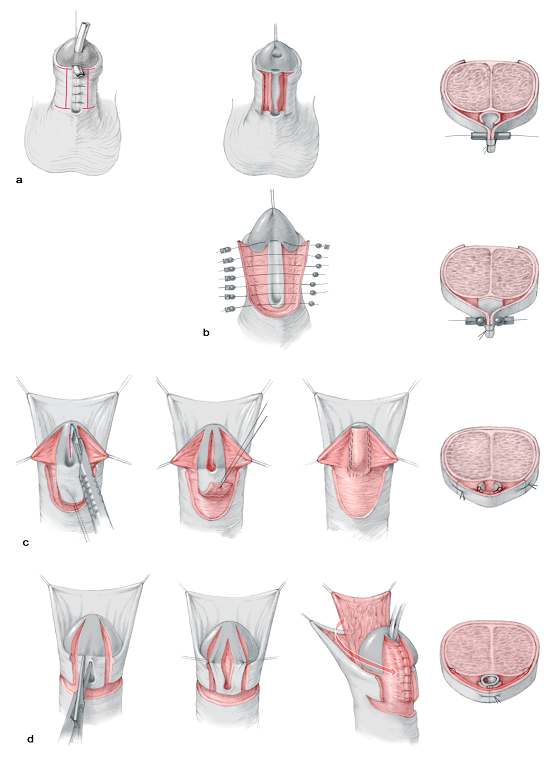
Anatomic classification of hypospadias recognizes the level of the meatus without taking into account curvature. A more recent classification was described. This classification indicates the site of urethral meatus (before and after chordee correction), the prepuce (incomplete or complete), the glans (cleft, incomplete cleft or flat), the width of urethral plate, the degree of penile rotation if present and the presence of scrotal transposition (Fig. 1, 2). Using the general classification (Fig. 4), surgeons are able to conduct multi-centre studies to evaluate different techniques of repair.
|